As an anxious person, COVID-19 is doing a number on me. My worries range from “That’s real” to “I can probably work that out” to “that’s not a thing.” Like: When will I see my parents again, in real life? Or, what will happen if my dog develops a UTI, now that her vet is closed except for emergencies? And, how will they film a new season of The Real Housewives of Anywhere in the Age of Social Distancing? There is one thing that I am literally praying for, though. Which is that my cystic acne from last year doesn’t come back until we’re securely in a post-COVID world. And that’s because if it does, I can’t get my medication — isotretinoin — here in the U.S.
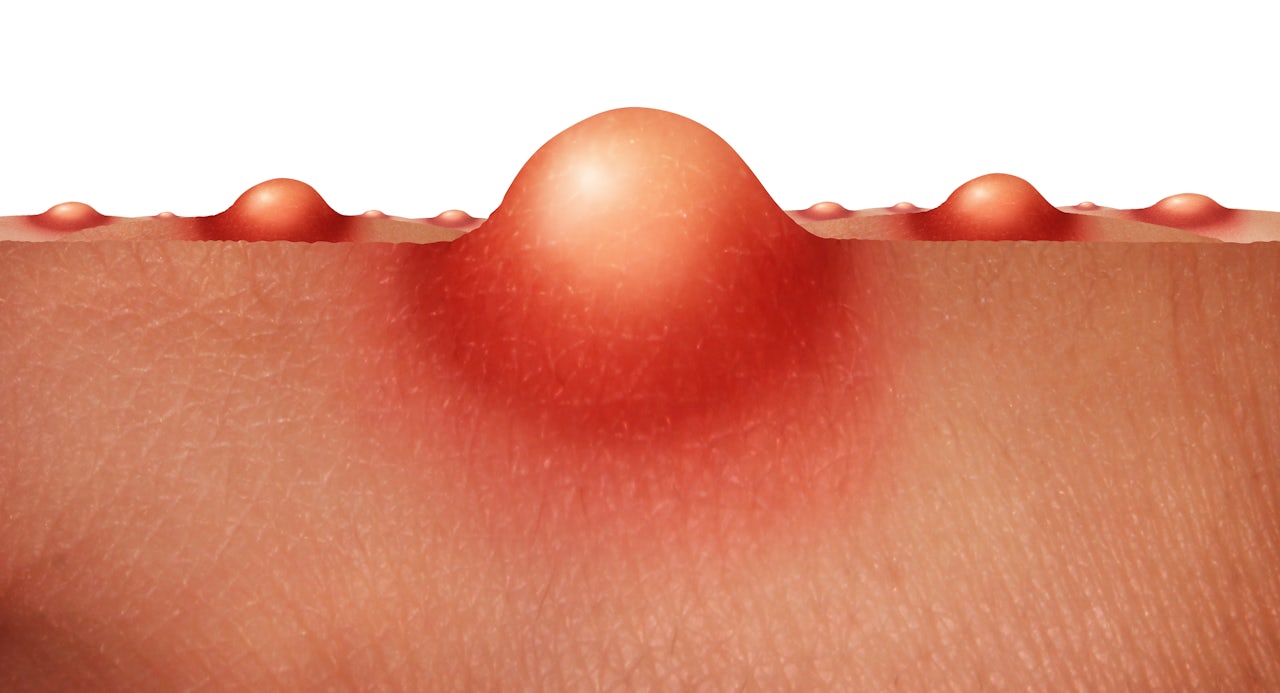
As a teen, when my peers struggled with acne, I waltzed around with nary a spot on my face. This blessed state came to a halt when the karma-collector came knocking around my 29th birthday. A red zit formed on my left cheek, so big it could’ve had its own gravitational force. Soon, it was orbited by a galaxy of throbbing, painful, pus-filled, bloody cysts. At a dinner, I wept to my friend, whose face contorted with the effort of lying to me. “It’s not thaaat bad!” she said. My mother begged me on FaceTime to stop picking at the unseemly constellation. My husband cropped his beard closer to his face, lest one of his hair-skewers detonate one of the painful stars. They took months to implode, leaving craters and scars in their wake.
The acne was diagnosed as cystic in my first visit to the dermatologist. I needed serious medication: isotretinoin, a chemical derivative of vitamin A, known by its former brand name, Accutane and sold today as Absorbica, Claravis, Amnesteem. Isotrentinoin is a miracle drug for many; studies show that 85 percent of patients who use it go into acne “remission.” But from costs, to delays, and onerous regulations, the process of obtaining a prescription for isotretinoin was arduous, even impossible. I am not alone in my experience; the barriers to obtaining isotretinoin have created a veritable black market for the drug. Eventually, when I ran out of options to obtain isotretinoin domestically, I traveled more than 7,000 miles to India, where I have family, for a prescription. This was already a completely unreasonable method of getting isotretinoin, and now it’s something I can’t do for the foreseeable future because of the pandemic.
Isotretinoin is a teratogen, meaning it can cause birth defects in babies, including cleft palates and congenital heart deformities; some babies do not survive pregnancy, as the drug drastically increases the risk of spontaneous miscarriage. In 1988, scientists at the Food and Drug Administration recommended that the drug be taken off the market because of observed birth defects. In a 2002 Harvard Law School paper titled “Babies, Blemishes and FDA: A History of Accutane Regulation in the United States,” a medical geneticist told authors Julia Green and Peter Hutt that “there is no other medication that poses an absolute risk anything remotely close to this, even medications used to treat cancer during pregnancy.”
The FDA had to find a way to eliminate fetal exposure to isotretinoin while still making the drug available to those suffering from acne. In 2002 it established the System to Manage Accutane Related Teratogenicity (SMART) that was deemed a failure. The program, which required female Accutane users be on two forms of birth control and produce two negative pregnancy tests before starting the drug, relied on doctor-patient consultations about the risks of Accutane and was weakly enforced; it neglected to ensure compliance from doctors and pharmacists as more and more patients were prescribed the drug.
Isotrentinoin is a miracle drug for many; studies show that 85 percent of patients who use it go into acne “remission.”
Computer-based iPledge was developed in 2006 by the FDA and the drug’s four manufacturers in order to right SMART’s perceived wrongs. Compared to SMART, iPLEDGE is strictly enforced. Non-compliance by dermatologists and pharmacies can lead to their suspension, and temporary or even permanent deactivation from iPLEDGE, meaning that they would not be able to prescribe or sell isotretinoin.
iPLEDGE requires the participation of doctors, patients, and pharmacists and mandates that female patients commit to two forms of birth control, which they need to have been taking for a month before starting treatment (abstinence is an acceptable birth-control method). This also applies, bizarrely, to women who have had their tubes tied and young non-menstruating girls. Prescriptions are refilled only on submission of monthly negative pregnancy tests, and if one is not picked up within seven days of the test, patients risk getting “locked out” of their eligibility for the drug. Then they must suffer through the exhausting bureaucratic exercise of “re-qualifying” for the medication. This is especially onerous for people living in rural areas, where not all pharmacies carry isotretinoin.
The requirement of double birth control was the biggest put off for me for taking isotretinoin. I was on the pill for about a year in my mid-20s and it made me depressed. The experience was so scarring that I wanted nothing to do with hormonal birth control ever again. Gynecologists dismissed my experience, conceding that birth-control induced depression happens to a “small percentage of women,” despite the growing mountain of evidence about the causal link between the two. I remember my dermatologist furrowing her brow when I expressed reluctance to get on hormonal birth-control or get a Long-Acting Reversible Contraceptive (LARC) like an IUD. I assured her that my partner and I used condoms, and had no plans to have biological children in the foreseeable future. Sympathetically, she said that due to iPLEDGE, her hands were tied.
Dermatologists have voiced concern about iPLEDGE’s demands. In 2006, the American Academy of Dermatologists (AAD) said that patients would find the system onerous, that it would complicate dermatologists’ ability to prescribe isotretinoin and care for their patients, compromising these relationships and changing the practice of dermatology. They were right. iPLEDGE’s stringent controls and complicated procedures effectively turned it into a drug of last resort for some dermatologists. While some patients have had little trouble getting it prescribed, others told me that they had to wait for long periods — from several months to years — before obtaining isotretinoin. Almost $700 and 10 months after her first appointment, Laura* is still waiting for her prescription. “I've tried antibiotics, tretinoin, spironalactone, and all sorts of salicylic acid topicals,” she said. “I missed a chance to obtain it several months ago because the process was so complicated and the office wasn't getting back to me with answers to my questions. Now my new dermatologist wants me to try it, and I have to go through another waiting period to make sure I don’t have a secret baby growing in me this time, either.”
iPLEDGE’s stringent controls and complicated procedures effectively turned isotrentinoin into a drug of last resort for some dermatologists.
My dermatologist said I’d have to take a six-month course of the antibiotic doxycylene before I could get Accutane. But I was battling a series of gastrointestinal issues and any antibiotic course would’ve decimated my gut. According to Pittsburgh-based dermatologist Dr. Laura Ferris, a reasonable trial of topical and antibiotic treatment lasts around three months, with oral contraceptives and/or spironolactone for women. “Some with severe inflammatory disease need to go straight to isotretinoin. This should be a decision made by a dermatologist and patient,” she said. I left my dermatologist with a week’s supply of doxycyclene, taking one before walking into Duane Reade, where I learned that my insurance wouldn’t cover it, and that a three-month supply would would cost me $500. She’d also warned me that that insurance might not be much help in covering the cost of Accutane. Stunned, I sat on a bench, my acne-ridden face wet with tears that made it burn.
Would I be this way forever? My face was in a constant state of what can only be described as “throbbing fire.” I never knew what would cause the cysts to explode — sometimes literally — with pain. A strand of my own hair, the pressure from holding a plank, the affection of my dog. I learned to sleep vampire-style: on my back, arms crossed on my chest, because even the softest pillow would irritate my cheeks. I couldn’t recognize myself in the mirror. I became an emotional and psychological wreck, and my confidence plummeted. I’d cake my face with foundation, dabbing cloud-paint or whatever Glossier said looked “natural,” before washing it away immediately, streaming gingerbread-colored tears into the sink. My dewy-skinned therapist kept assuring the anxious mess of me that There were remedies! That medicine has come a long way! but, at each turn, roadblocks presented themselves. My grandmother cursed those whose “evil eye” had caused my skin to erupt. It wasn’t just that I had to wait patiently, I also had to commit to a LARC or hormonal birth control, which would have submerged me deeper into depression. I also didn’t want to be coerced into inserting an IUD. I had been diagnosed with cystic acne and needed medication to treat it, and yet I couldn’t get it.
In the depths of my despair, I poked around internet acne support groups, quickly finding posts discussing how and where to get isotretinoin online. Without a prescription. Companions-in-misery shared names of online pharmacies that sold authentic medication, detailing how to go about getting it. Even when mods banned these discussions, archived posts remained available. I even found a “buyer bible” on how to buy isotretinoin on the dark web — which I’d only thought of as a haven for arms dealers and Bitcoiners. Cursory Googling led me to a host of pharmacies based in Canada and the UK that shipped generic Accutane to the U.S. in “discreet packaging.” These pills are often heavily discounted, available in doses from 10mg to 40mg. I placed isotretinoin in my cart a hundred times, filling in my CVV, my address… until immigrant-panic of being caught held me back.
From 2006 to 2007, the emergence of such pharmacies caused concern among public health and government officials. Dermatologists guessed that then newly implemented iPLEDGE caused the proliferation of such bootlegging operations. In 2014, Dr. Neal Bhatia wrote an article for Practical Dermatology about isotretinoin’s ubiquity online, listing ways to protect prescribers and patients. (I reached out to Bhatia to talk about it, but he declined to comment.) A 2014 study in the journal Pharmacoepidemiology and Drug Safety found that isotretinoin could be purchased from 42 sites without a valid prescription. The researchers attempted eight purchases; seven that arrived were all verified as isotretinoin. While they purchased isotretinoin from pharmacies in Europe, Russia and the U.S., they found that the drug itself originated in India, where it was a fraction of the cost. As soon as I learned that my birth land was the origin for cheap acne medication, I called my mother, desperately asking her to find people to be Accu-mules for me. She wouldn’t allow it, but promised that we would see a dermatologist when I next visited India.
I learned to sleep vampire-style: on my back, arms crossed on my chest, because even the softest pillow would irritate my cheeks.
It’s unclear how many people buy isotretinoin online. The FDA told me they don’t track these numbers; no one, as far as I can tell, has been caught. While none of the dermatologists I spoke to about this had observed anyone obtaining isotretinoin online, Ferris acknowledges that challenges in obtaining it legally is the likely cause. “The cost of the drug itself may be prohibitory to some patients,” Dr. Joshua Zeichner, a dermatologist in New York City, told me. One person who bought Accutane online told me they did so strictly for this reason. Isotretinoin’s high costs have the greatest impact on women of color, who have lower rates of insurance than white women. One study found that black patients receive less oral isotretinoin than white patients, and that its price appeared to be a key factor in this difference.
I landed in India eight months after zit zero appeared (acne time feels like dog years) I saw the dermatologist that very day and he prescribed isotretinoin immediately. Accutane would cost me $7 monthly. I signed a paper stating I was informed of the drug’s effects and the risks of getting pregnant. That was it.
iPLEDGE, while designed to protect those who take isotretinoin, hinders access to people who need this drug, especially people of color, those in the LGBTQ+ community, and the poor. A study published in the journal PLoS One last year shows that nonwhite patients are 50 percent more likely to end their isotretinoin course earlier than white patients, with iPLEDGE-related barriers being the most commonly specified reasons. iPLEDGE can be humiliating for queer women, forcing them to comply with birth control regulations they wouldn’t otherwise need, and triggering for trans men, who can experience severe acne with testosterone treatment. What also goes unacknowledged is that iPLEDGE’s birth-control requirements are particularly discouraging for women of color, who face numerous barriers to accessing contraception and are less likely to use effective contraceptive devices such as hormonal methods or LARCs. A violent national history of racism, eugenics, health care providers’ pressure to use birth control, and reproductive coercion — including forced sterilizations — has destroyed black, Hispanic, and Native American communities’ trust in the health care system. A nationwide trend of state bills in the ’90s incentivized or even required women receiving public benefits to get a LARC. So, while LARCs are widely recommended for iPLEDGE, this history (and the exorbitant costs: starting an IUD can cost a month’s salary for a woman working full time at minimum wage) can justifiably make women of color reluctant to opt for a medicine that could help them greatly.
I’d cake my face with foundation before washing it away immediately, streaming gingerbread-colored tears into the sink.
Crucially, iPLEDGE infantilizes and distrusts women, prioritizing prevention of teratogenic side-effects at the expense of others. As a kid I studied in an all-girls convent in India, that had a daily policy of checking if we wore bloomers under our uniforms until we were 13. Demurely, we’d lift the hem of our skirts, showing monitors a sliver of the unsightly, turn-of-the-twentieth-century undergarment. iPLEDGE feels like bloomer-checking 2.0. Its control over women’s bodies is completely out of place in a society that ostensibly guarantees bodily autonomy. It imposes all the wrong responsibilities on patients like 7-day prescription pick-up windows, instead of trusting them to make decisions in their best interests.
Access to medication shouldn’t be about luck or resources, and people shouldn’t be tempted to buy it from unregulated, potentially unsafe sources. We also shouldn’t have to go to India to get isotretinoin (even if off-season flight tickets before coronavirus and isotretinoin’s price there can arguably be a cheaper and less onerous alternative). When I look at pictures of my former painful Jackson Pollock-painting face, I can hardly believe it. I don’t have to slather my face with foundation anymore, and fading cystic constellations pepper my cheeks like freckles. Recently, a bartender told me they were “super cute.”